Role of Private Enterprises in making Government Healthcare Services Better
Health is a basic requirement and right of every human being. Providing effective healthcare is an essential contribution towards the social and economic development of a nation which in turn brings economic sustainability and growth. Healthcare systems globally face huge challenges in delivering high-quality, accessible, and affordable care, in particular to the growing population in rural and remote areas.
Various Healthcare Models across the Globe
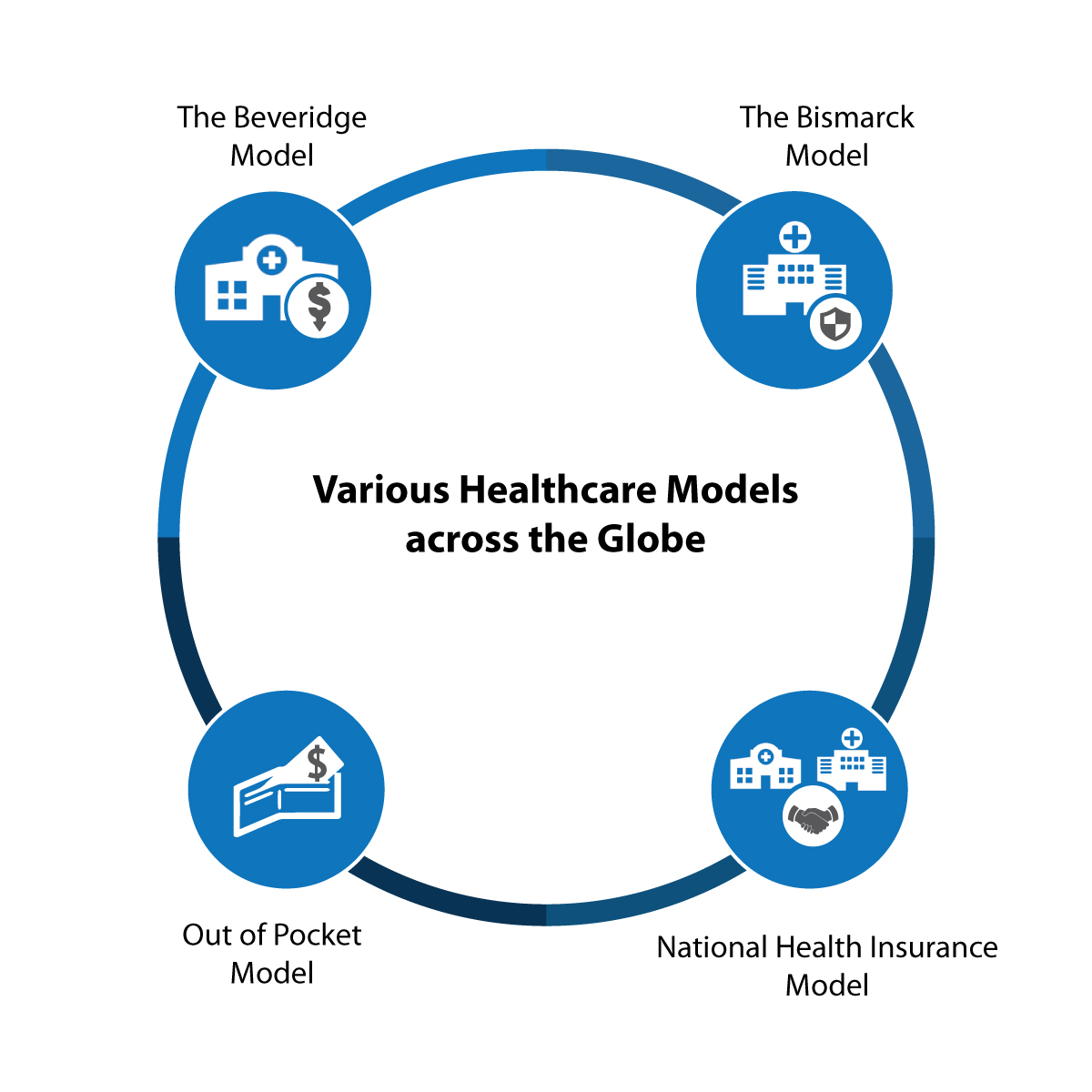
There are 195 countries in the world today, and each country has its own set of arrangements for meeting the basic goals of its health care system. In general healthcare systems have four basic models:
- The Beveridge Model: In this model health care is provided and financed by the government through tax payments. In this model, many but not all hospitals and clinics are owned by the government. The cost of treatment in this model tends to have low costs per capita, because the government, being the sole payer, controls what doctors can do and what they can charge. It is the purest example of total government control. Great Britain, Spain, most of Scandinavia and New Zealand are a few countries that follow “Beveridge Model”.
- The Bismarck Model: This model uses insurance system which is financed jointly by employers and employees through payroll deduction. Private hospitals and clinics are the major players in this model. Bismarck model is found in Germany, Belgium, France, Netherlands, and Japan.
- National Health Insurance Model: National Health Insurance Model has elements of both Beveridge and Bismarck model. This model uses private sector providers for various healthcare needs, but the payment comes from the government-run insurance program that every citizen pays into. Since there’s no need for marketing, no financial motive to deny claims and no profit, these universal insurance programs tend to be cheaper. The classic NHI system is found in Canada; Taiwan and South Korea have also adopted this model.
- Out of Pocket Model: This model involves direct payments made by individuals to health care providers at the time of service. This model excludes prepayment of health services in the form of taxes, health insurance premium or any reimbursements. Unregulated direct charges often constitute a major access barrier contributing to high out-of-pocket payments. Developing nations such as India, Pakistan, Srilanka, Bangladesh and parts of Africa fall within this model.
Healthcare Models in Developed vs Developing Economies
Healthcare models in the developed world typically emphasize on the implementation of technologies, end of life issues, and issues such as substance abuse, however, on the other hand developing nations still struggle for basic primary care.
Lack of transparency, under-utilization of existing resources and accountability are a few key factors that contribute to this scenario.
In 2003, a Lancet study reported that 63% of child deaths in the 42 countries that account for 90% of global child mortality could be prevented each year through more effective primary care.
Although healthcare in developing countries has undeniably improved when compared to the 90’s, there is still much to be done. Previously primary healthcare was limited to physical examination but in today’s era, primary healthcare practices are equipped with various diagnostic facilities. Easy access to primary health care and diagnostics undoubtedly can reduce the number of hospitalizations; increase life expectancy and thereby can lead to better overall health for the community.
Technology as an Enabler
Technology has had a significant impact on the field of healthcare, be it in its simplest form as Telemedicine and Teleradiology or complex end high procedures such as Robotic surgeries; Laparoscopic surgeries, Bionic limbs, etc. Teleradiology and Telemedicine being at the forefront of technology adoption have helped transform unsustainable healthcare systems into sustainable ones, by providing an affordable, faster and effective solution. With Telemedicine, gone are the days when the physical presence of a doctor was required for treating patients. Video-based telemedicine has helped doctors, diagnose, monitor and treat remotely located patients in real time, using equipment that can extend from basic video conferencing to a full-fledged suite of telemedicine scopes and devices.
Value of Private Enterprises in Delivering Healthcare
In most developing countries, the Government is responsible for ensuring basic health for its citizens but at a very rudimentary level. However as one proceeds higher up the value chain for more complex procedures, not many government hospitals have the right equipment and right expertise. Despite thin margins, the private healthcare sector plays a major role delivering healthcare. Owing to reasons such as availability of technology and expertise; ease to access; private ventures (profit and non-profit organization) are increasingly becoming the center for high-quality healthcare services. But due to their exorbitant costs, only a limited section of the society can avail these services. The need of the hour is to create the balance and find the sweet spot between the private enterprises making the technology and the expertise available with the government which has the infrastructure and scale thereby enabling universal access and making the cost lower. Doing so will ensure that the utilization of every dollar spent by the government is maximized while ensuring that the quality remains the same.
PPP models in China
Over the last decade, China has stepped up promotion of PPP models as a way to help improve healthcare provision. As a result of sustained endeavors, PPP in China has increasingly become a popular feature of the healthcare industry.
Beijing New century International Children’s Hospital PPP model
Beijing New century International Children’s Hospital manned by highly qualified doctors and the staff was the first specialized children’s hospital to operate by international standards. This PPP model was dedicated to providing comprehensive and quality healthcare service to newborns, infants, school children, and teenagers. It has yielded a range of complimentary benefits thereby enabling efficient use of resources to better serve patients with more targeted care.
Phoenix Healthcare Group
This PPP model focused on building a network of treatment, healthcare, and emergency medical service. This model was aimed to overcome inefficiencies of the old system and to bring in rapid progress in meeting special healthcare needs.
PPP healthcare models in India
According to a recent report “India will end up with a total bed density of 1.84 per 1,000 people against the global average of 2.9 and WHO guideline of 3.5 in 2022”. These figures scream out the fact that while on the one hand the public health systems must be strengthened at all levels for a better service, healthcare needs to be supplemented through active private sector participation too.
A PPP model ensures this by scaling up the capabilities of public hospitals to maximize their impact and reach.
To tackle healthcare delivery head-on, the government needs to understand and take up the responsibility of either being a provider or a payer. If as a provider, the government should contribute to building infrastructure, equipping machinery and managing operations or, if it wants to be the payer it pays for the healthcare services that are provided by the private hospitals.
India has a long history of PPPs in health with most of the National Health Programmes partnering with non-profit and for-profit organizations.
Assam Teleradiology Project of NRHM With Healthfore Technologies
This PPP model was aimed to make radiology services accessible and affordable to the entire rural populace of Assam.
Karnataka Integrated Tele-medicine and Tele-health Project
This PPP model facilitated the investigation by specialists after preliminary examinations which aided in timely diagnosis and treatment for the patient. With the help of telemedicine, access to areas that were under-served or un-served was made easy. It improved specialty care and reduced both time and cost for rural and semi-urban patients.
Other Government and private joint Ventures
Teleradiology Solutions & Singapore Government
Teleradiology Solutions was accredited by the Singapore Ministry of Health to provide teleradiology services to hospitals and diagnostic centers in Singapore. This joint venture had dramatically reduced the report turnaround time from 2-3 days to less than an hour.
Teleradiology Solutions & Tripura Government
This venture helps patients at any of the government-run community and primary health centers and hospitals have their X-rays contemporaneously interpreted in real time by a specialist radiologist at a central reporting center located in a different part of the country. This partnership has made remote radiology available to healthcare providers across Tier II and remote markets in India. This partnership was backed by a team of over 50 radiologists across multiple centers providing round-the-clock remote radiology reporting services. This initiative to this date has been a resounding success with more than 27246 reads till date across 23 sites in the state.